This session covers resuscitation of a young infant (who may be just a few days old but who has not just been delivered). There are a lot of similarities with neonatal resuscitation and the skills required are similar.
The resuscitation of the YI is very similar to the newborn, except for the initial stepsThe letters A and B in “ABCCCD” represent “airway and breathing”.
To assess if the child has an airway or breathing problem you need to know: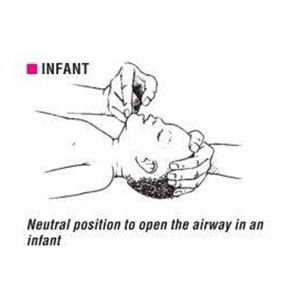
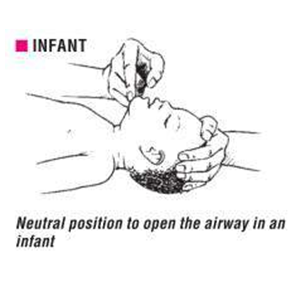
The neck is slightly extended and the head is tilted by placing one hand onto the child’s forehead.
Lift the mandible up and outward by placing the fingertips of the other hand under the chin.
| Conscious | Unconscious |
|---|---|
| Inspect the mouth and remove secretions | Open the airway with head tilt and chin lift |
| Let the infant assume a position of maximum comfor | Inspect the mouth and remove secretions |
| Give oxygen | Check if maneuver has improved air entry by looking at the chest |
| Continue assessment | If not, insert airway |
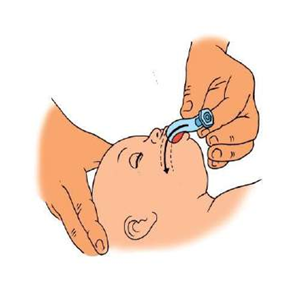
The oropharyngeal or Guedel airway can be used in an unconscious infant to improve airway opening. It may not be tolerated in a patient who is awake and may induce choking or vomiting. Guedel airways come in different sizes; an appropriate sized airway goes from the angle of the mouth to the angle of the jaw when laid on the face with the convex side up.
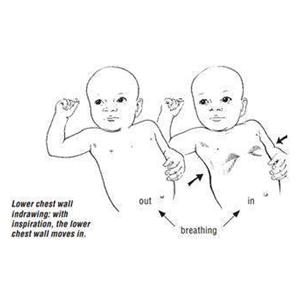
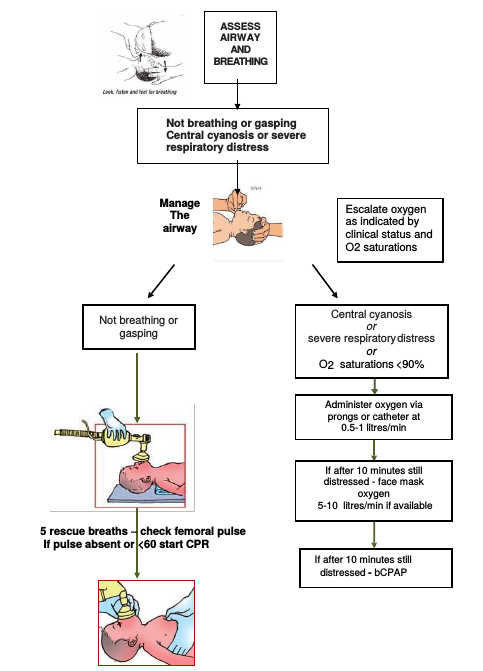
Is there difficulty in breathing while breastfeeding? Is the baby breathing very fast, has severe lower chest wall in-drawing, or using the accessory muscles for breathing which cause the head to nod with every inspiration? Are there any abnormal noises heard when breathing? A short noise when breathing out in young infants is called grunting. Grunting is a sign of severe respiratory distress.
Signs of severe respiratory distress
A baby with severe respiratory distress should be allowed to take a comfortable position of his choice and should be given oxygen. Oxygen may be provided with a catheter or prongs. If the baby’s breathing difficulty worsens or the baby has central cyanosis while on catheter or prongs: add oxygen at a high flow rate via a face mask (5 litres/min), if available.
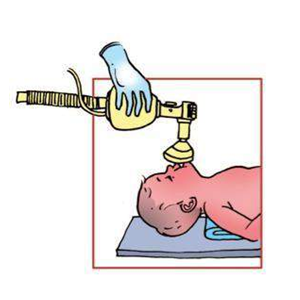
Ventilate with bag and mask (BMV)
If the child is not breathing even after the above manoeuvers or spontaneous ventilation is inadequate (as judged by insufficient chest movements and inadequate breath sounds), ventilate with a self-inflating bag and mask.During bag and mask ventilation it may be necessary to move the baby’s head and neck gently through a range of positions to determine the optimum position for airway patency and effectiveness of ventilation. A neutral position without hyperextension of the neck is usually appropriate for infants. Infants may need padding under the shoulder to prevent excessive flexion of the neck that occurs when their prominent occiput rests on the surface on which the child lies.
Call for help in any child who needs Bag and Mask Ventilation (BMV) since some of these infants may additionally need chest compression.
After five effective ventilations, check the pulse (femoral) for ten seconds. If pulse is absent, the second person should start chest compression.Note: while it is often possible to resuscitate a baby who has stopped breathing but still has a good heart beat i.e. a respiratory arrest, it is almost never possible to resuscitate a baby whose heart has stopped, i.e. a cardiorespiratory arrest.